Parasomnias
This field of sleep disorders and treatment can be overwhelming. It is our goal to provide you with the knowledge and resources to make it simple.
The term “Parasomnia” refers to a large range of sleep disorders that are typically not very frequent. Rarely will these occur to such a degree that medical help is needed. Most of these disorders are rare after childhood, so adults should seek medical advice. Links for details and examples of select parasomnias: Bruxism, Restless Leg Syndrome, Periodic Limb Movement Disorder, Nocturnal Seizures, Insomnia, and Fibromyalgia and Sleep.
It is my goal to provide you with enough information that you know what questions to ask your Sleep Disorders Specialist. Your sleep Doctor will be better able to answer questions about your particular problem.
Sleep Starts: Motor sleep starts are what most people have experienced when just about to fall asleep. It’s the sudden violent jerk that many describe as falling off a cliff. There are two other types of sleep starts. A visual sleep start is having a sensation of a blinding light when you are falling asleep. An auditory sleep start is a sensation of a loud snapping sound that seems to originate in your head.
Bruxism (Teethgrinding): Typically it is your dentist that will let you know you have this problem as the grinding will slowly wear down your teeth. Read more on Bruxism.
Sleep Talking (Somniloquy): Hmmm….how to describe sleep talking…..hmmm. It’s when you talk in your sleep. Unfortunately this is totally normal and no doctor is going to do anything about it because it has no medical significance. It is very fun to listen to in the sleep center though. If you have any secrets you don’t want to share, wearing a gag at night would be beneficial.
Rhythmic Movement Disorder: This occurs almost exclusively in young children. This involves head movements like headbanging and rolling. It also involves body rocking and can be accompanied by moaning.
Nocturnal Seizures: These only occur during sleep and can be detected with an all night sleep study with a seizure montage (doubles electrodes on the patients head for a near full EEG during sleep) These can mimic many other parasomnias with a person exhibiting yelling, crying, movement and talking. Nocturnal Seizures can be treated with medication. Read More about Seizures and see pictures.
Sleep Paralysis: This typically occurs when waking up from a dream (REM sleep). A person with sleep paralysis will experience an inability to move right after waking. This can be caused by being overly sleep-deprived or someone with narcolepsy. This isn’t dangerous, but it is extremely frightening.
Hypnagogic Hallucinations: This is dreaming while awake and occurs right before falling asleep. These “dreams” are often very scary in content, mostly because it’s set in reality. By this I mean that if you’re in bed and falling asleep, the hallucination involves you being in bed. It’s part reality and part…ta da…hallucination. These are often seen in people who have narcolepsy. These are often reported as being paranormal activities.
Rapid Eye Movement Behavior Disorder: (a.k.a.) REM behavior disorder. Patients with this will act out their dreams while asleep. These dreams are normally violent so the patient will punch and swing wildly. I have witnessed patients doing things such as fishing in their sleep though. This is when the normal paralysis that should occur during REM sleep doesn’t. This is most often seen in older men where the paralysis is non-existent or only partial. Unfortunately, a very high percentage of patients with REM behavior disorder develop Parkinsons Disease and Dementia. See below for an example of this.
Bruxism
Bruxism is the grinding of teeth during sleep. This typically occurs while in Stage 2, or N2, sleep. You can see the EMG signal increases (chin activity) and the tension throughout the EEG channels from muscle tension while grinding teeth.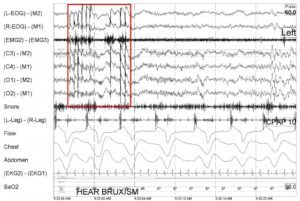
Dentists have found that 10-20% of patients have evidence of bruxism. Of those, about 10% have enough damage to their teeth to require treatment.
Bruxism can be caused by anatomical problems that may be corrected. Lesions in the central nervous system may be possible, though rare.
Realistically the best treatment is prevention of further damage to the teeth by wearing a bite guard. A dental examination would be needed for a custom made bite guard.
If you have a bed partner and you have bruxism, it is very likly that they have heard you grinding your teeth. The sound is AWFUL!
Resless Leg Syndrome
RLS means restless leg syndrome. It’s not a true sleep disorder because you aren’t asleep while it is occuring. This was popularized on Seinfeld as “The Jimmy Legs.” They should really make this the official name because it sounds way better.
Symptoms of RLS:
- Intense urge to move your legs.
- Unpleasant sensations in your legs that can be described as creeping, crawling, pulling, tingling, or electric.
- Symptoms get worse while resting or during periods of inactivity.
- Movement of your legs relieves the symptoms.
- Symptoms are worse in the evening or while you’re in bed.
To get a diagnosis of Restless Leg Syndrome (RLS) you will need to see a sleep specialist or a neurologist that has knowledge of RLS. Diagnosis is determined by your medical history and an examination. Tests that can assist in reaching a RLS diagnosis include blood tests and an overnight sleep study. Typically RLS symptoms are easily found by answering the following questions.
In treating Restless Leg Syndrome it is important to see if there may be other medical conditions associated to the problem. These include: diabetes, iron deficiency anemia, arthritis, and the use of some medications.
Treatment of these conditions may resolve RLS.
Some RLS isn’t caused by diabetes, iron deficiency anemia, arthritis, or medication. If this is the case with you, then there are some home remedies that can be attempted to help with occasional episodes of RLS.
You can try: hot baths before bedtime, leg massages, heat, ice, asprin, regular exercise, or eliminating the consumption of caffeine. Probably the best over the counter drug you can use to treat both RLS and PLMD is Manganese. 10mg of this appears to have a strong effect on decreasing the creepy crawling feeling caused by Restless Leg Syndrome.
If home remedies don’t help with RLS, then you may need your physician to prescribe medication to help. Sometimes this involves eliminating medication that may be causing the RLS. It is VERY IMPORTANT to have a physician monitor medication changes.
Medications that can TREAT RLS: I-dopa/carbidopa (Sinemet), pergolide (Permax), pramipexole (Mirapex), ropinirole (Requip), conazepam (Klonopin), gabapentin (Neurontin), codeine, and propoxyphene (Darvon). Best non-prescription drug that is effective is an over the counter Manganese supplement as well as Magnesium (though Magnesium is plentiful in most diets. This supplement can be highly effective at calming your legs when trying to get to sleep.
Medications that can WORSEN RLS: amitriptyline (Elavil), fluoxetine (Prozac), antidepressants, (Benadryl), cold and allergy medications, prochlorperazine (Compazine), metoclopramide (Reglan), lithium (Eskalith, Lithobid, Lithonate, Lithotabs), haloperidol (Haldol) phenothiazines (Mellaril, Thorazine).
Nocturnal seizures are a form of epilepsy caused by abnormal electrical activity that can be caused by lack of sleep, head injuries, alcohol, stress, hormones, brain infections, and recreational drug use.
Most people suffering from nocturnal seizures have epileptic seizures during the day. If the cause of the seizures can be identified, it is possible to control the nocturnal seizure.
Symptoms are difficult since mostly they manifest as movements during sleep and usually last under 30 seconds. Other clues may be wetting the bed and waking with a bloody mouth from biting the tongue.
If nocturnal seizures are suspected, consult a neurologist. An overnight sleep study at a local clinic with video monitoring can be helpful. See the example of a nocturnal seizure during a sleep study above.
Insomnia is an inability to fall asleep or to stay asleep as long as desired. The only way that insomnia can really be diagnosed is through a polysomnogram (sleep study) to show evidence of difficulty in initiating and maintaining sleep. A more practical definition (and a cheaper diagnosis) of insomnia is a positive response to either: “Do you experience difficulty sleeping?” or “Do you have difficulty falling or staying asleep?”
Insomnia can accompany several sleep, medical, and psychiatric disorders characterized by a persistent difficulty falling asleep and/or staying asleep or sleep of poor quality. With this, there is a clear difficulty in functioning during the day. Insomnia can be short term (about a month) or long term (longer than a month). This can lead to memory problems, depression, irritability and an increased risk of heart disease. It will also lead to you being incredibly pissed of and frustrated.
Insomnia can be classified as transient, acute, chronic, and another that I add….CPAP induced insomnia.
Transient insomnia lasts for less than a week. It can be caused by another disorder, by changes in the sleep environment, fighting your natural sleep cycle, depression, or stress. The symptoms of transient insomnia are the same as sleep deprivation.
Acute insomnia is the inability to consistently sleep well for a period of less than a month. Insomnia is present when there is difficulty initiating or maintaining sleep or when the sleep that is obtained is non-refreshing or of poor quality. This occurs despite the insomniac having all the time in the world for sleep along with the right conditions for sleep. Acute insomnia is also known as short term insomnia or stress related insomnia. I’ve suffered from this and have a blog post on the experience….a miserable experience at that!
Chronic insomnia lasts for longer than a month. It can be caused by another disorder, or it can be a primary disorder. In the sleep disorders field, chronic insomnia is very often some form of sleep apnea. The most frustrating of these is UARS (upper airway resistance syndrome) since many labs lack the ability to detect this subtle collapse of the upper airway. This causes the insomniac to go undiagnosed and don’t get the validation that they need to treat their insomnia. People with high levels of stress hormones or shifts in the levels of cytokines are more likely to have chronic insomnia. Some people with chronic insomnia (or sleep apnea) will describe their life as living in a fog.
CPAP induced insomnia is something that the medical community isn’t aware of “officially”, but anyone new to CPAP is well aware of. This could fall into two different categories of insomnia, Acute and Chronic.
The CPAP induced insomnia could be acute if the root of the insomnia is the anxiety over the new diagnosis of “sleep apnea” along with all the lifestyle changes that come with it. These include possible stigmas attached to using PAP therapy as well as feelings of having your private sleep space invaded by a foreign machine and mask. Cognitive behavioral therapy can be very helpful in getting through these negative feelings.
The CPAP induced insomnia could be chronic if the problems sleeping with a PAP machine and mask is caused by your apnea not being treated completely. This is very often from undiagnosed subtle sleep disordered breathing (UARS) that is still persistent though the apneas and hypopneas have been successfully treated.
What to do about your insomnia? First thing to do is exactly what you’re doing….educate yourself. Now that you have a foothold on this you need to take this to your physician for their professional opinion. Depending on the cause of your insomnia, the fix can be phychotherapy for stress, medications to alleviate anxiety, or CPAP therapy if sleep disordered breathing is the cause. A sleep disorders study may be a good option to validate your concerns. In the meantime, you can join our free forum (click the icon below) to discuss your concerns with other people that have been in your shoes and gotten through their bout of insomnia.
Fibromyalgia (Fibromyositis; Fibrositis)
Fibromyalgia is a syndrome that causes long term body pain and tenderness in joints, tendons, and muscles. It seems to effect mostly women between the ages of 20 and 50.
Some of the symptoms of fibromyalgia appear to be headaches, depression, anxiety, fatigue, and (most interesting to me and my line of work) sleep problems.
The cause of fibromyalgia is unknown, but it appears that physical and/or emotional trauma may be a trigger. Other triggers may be an abnormal pain response. The final possible trigger appears to be sleep disturbances. In the sleep lab, one of my jobs is to score sleep studies where I go over the raw wave forms that have been collected during the night.
I rarely look at the patient chart prior to scoring the sleep stages and respiratory channels because I feel it can cause bias. I can accurately predict whether or not a patient has fibromyalgia based
on how their Delta (Stage 3, or N3) sleep appears. I find this to be fascinating. Is this a symptom of fibromyalgia, or a cause of it? Should a sleep study be used to diagnose fibromyalgia? See examples below and you can compare child delta, adult delta, and adult delta in a patient diagnosed with fibromyalgia.
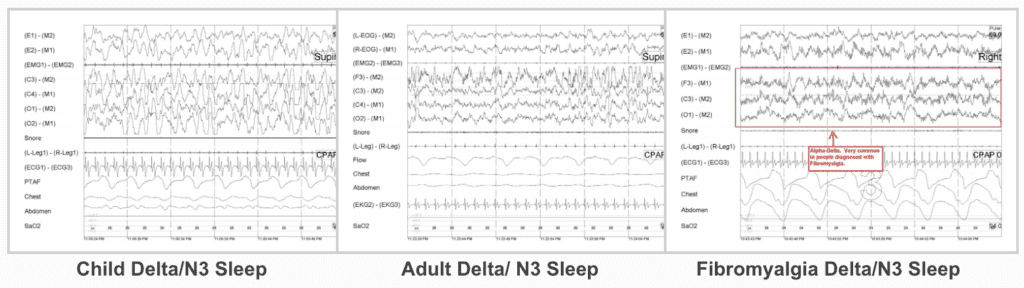
It is the Delta sleep of a child. It doesn’t get any bigger or more beautiful. This is why you can seen a marching band through the room of a sleeping child in Delta and they won’t budge. The middle example is an adult in Delta. It also looks nice, but the decrease in human growth hormone released as we age causes the waves to attenuate. The example on the right is the Delta of a female that has been diagnosed with fibromyalgia. Even the untrained eye can see the difference.
Alpha-Delta is seen in the fibromyalgia patient. Delta should be slow waves in the range of .5 to 2 Hz (cycles per second). This is supposed to be when our body repairs itself so we wake feeling physically refreshed. In patients with fibromyalgia we see several bursts of Alpha waves, 8 to 12 Hz (cycles per second). Is this why the fibromyalgia patients have pain? Is it because the body isn’t able to properly heal itself during the night? This is my theory. Questions? Click below and join my forum. Let’s talk about it.
Pain is the main symptom of fibromyalgia and can be mild to severe.
The painful areas are called tender points. These can be found all over the body and can range from a deep ache to a shooting burning pain.
People with fibromyalgia seem to wake up with stiffness and aches that may be related to their Alpha-Delta sleep. Sometimes this pain improves during the day and then worsens during the night. Others seem to have pain all throughout the day.
If you feel that you have fibromyalgia, please contact your doctor. Unfortunately this is no known way to prevent fibromyalgia from occurring, but it may be helpful to join a support group that specializes in the subject.
Periodic Limb Movement Disorder
PLMD stands for Periodic Limb Movement Disorder, though many people call it periodic leg movement disorder. This isn’t the worst thing ever since it primarily effects the legs (sorry arms)
To get a diagnosis of Periodic Limb Movement Disorder (PLMD) you will need to see a sleep specialist and have a Sleep Study (Nocturnal Polysomnograph.) During a sleep study electrodes are placed on the front of your shin. They’re placed over the Anterior Tibialis so that when you move your leg, they are triggered and we (sleep techs) get a signal. For a PLMD diagnosis the leg movements must:
- Last at least 0.5 seconds, but no longer than 10 seconds.
- Occur during sleep.
- Not occur during a sleep disordered breathing event.
- Movements must be separated by at least 5 seconds, but no more than 90 seconds. You need 4 movements without arousals or sleep disordered breathing which counts as 1 PLM. An index of 5.0 PLM (per hour of sleep) get a diagnosis of PLMD.
Confusing? You betcha!!!! How about a picture. It’s worth at least a couple of words……
 To the left is a 2 minute segment. The patient is in sleeping. The spikes in the L-Leg-R-Leg channel are leg movements. They are about 15-30 seconds apart. No sleep disordered breathing is present. No arousals are present. This is a clear example of Period Limb Movement Disorder.
To the left is a 2 minute segment. The patient is in sleeping. The spikes in the L-Leg-R-Leg channel are leg movements. They are about 15-30 seconds apart. No sleep disordered breathing is present. No arousals are present. This is a clear example of Period Limb Movement Disorder.
Medications that can TREAT: Dopaminergic Agents, Opioids, Benzodiazepines, and Anticonvulsants are the four classes of drugs used to treat PLMD (and RLS). The best option to try first is 10mg of over the counter Manganese. This supplement can be highly effective at calming your legs when trying to get to sleep. The same can be said of Magnesium, though it is more plentiful in most diets. Give it a try as well.
Typically PLMD is usually not treated with medication unless Restless Leg Syndrome has also been diagnosed.
Sleep Services
Speak with a Sleep Technologist about your questions about CPAP, APAP, Bilevel, or ASV Therapy.
Sleep Testing
At home diagnostic sleep testing equipment rental for testing in your own home.
CPAP Masks & Accessories
Get In Touch
We are here to help you with any of your sleep diagnotics needs. From at home sleep testing, to CPAP assistance, to sleep advice, we are happy to help you in any way we can. Questions about our services? Please don’t hesitate to contact us.



